Eye on Women’s Health
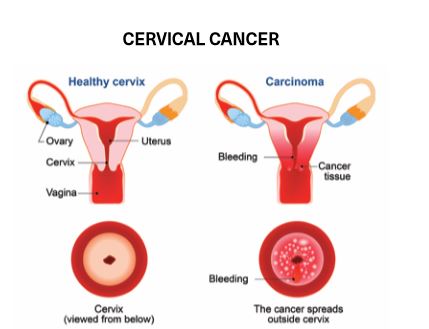
Cervical cancer screening saves lives.
 The American Cancer Society estimates that 13,240 cases of invasive cervical cancer will be diagnosed in the United States in 2018. Due to early detection of cancer through cervical screening tests, the cervical cancer death rate has decreased annually since 1975.
The American Cancer Society estimates that 13,240 cases of invasive cervical cancer will be diagnosed in the United States in 2018. Due to early detection of cancer through cervical screening tests, the cervical cancer death rate has decreased annually since 1975.
Dr. Brianne Anderson who specializes in OB-GYN at Crescent City Physicians, Inc., a subsidiary of Touro Infirmary, explains the importance of cervical cancer screening. “The main cause of cervical cancer is HPV (human papillomavirus) and with regular screening tests, like the Pap smear and the HPV DNA test (HPV test), we can save lives,” she says. “Cervical cancer often does not cause symptoms until it is advanced; that is why it is important to get screened even when you feel healthy.”
THE PAP SMEAR
According to the Centers for Disease Control and Prevention, the Pap smear (or Pap test) is one of the most reliable and effective screening tests for cancer. During this test, a speculum is inserted into the vagina to gain access to a woman’s cervix and to take a sampling of cells. If the cells from the cervix are abnormal, your doctor will create a treatment plan to prevent cancer from developing. “Nothing is 100 percent but the Pap smear opens the door to investigation,” Dr. Anderson says. “It is important to have regular cervical screening tests, because abnormal cells could turn into cancer over time. The recommendation is that all women should start getting regular Pap smears at age 21. This test can be slightly uncomfortable but is generally not painful.”
THE HPV TEST
HPV is the most common sexually transmitted infection in the United States, affecting about 14 million people each year. Common among sexually active individuals, HPV can cause health problems such as pre-cancerous cells and genital warts.
The Pap smear and HPV tests look for different things. The Pap smear checks your cervix for abnormal cells that could turn into cervical cancer, and the HPV test checks your cervix for the virus (HPV) that can cause abnormal cells and cervical cancer. The HPV test is used along with the Pap smear (referred to as co-testing) when testing women aged 30 and older or on women aged 21 to 29 with abnormal Pap smear results. “Although HPV infections are fairly common, most people will have a transient infection,” Dr. Anderson says. “HPV is found in a majority of cancer cases, but most cases of HPV do not become cancerous. There are different strains of the virus, and some strains have a higher association with cervical cancer. It is these strains that we look for with the HPV test.”
GUIDELINES
The American Cancer Society recommends the following:
At the age of 21, a Pap smear and cervical cancer screening.
Women aged 21 to 29 years should have a Pap smear every 3 years.
From age 30 to 65 years, women should have a Pap smear every 3 years and a Pap smear and HPV test every 5 years.
After the age of 65, women whose tests have shown clear results in the past 10 years can stop screening. If tests show pre-cancer, screening should continue until 20 years after the date the cancer was found.
Women with a high risk of cervical cancer should undergo screening more often.
ABNORMAL TEST RESULTS
When both the Pap smear and the HPV test results are abnormal, a colposcopy is used to take a closer look at your cervix and to biopsy any abnormal areas. Further testing and/or a treatment plan will be based on the results.
Cryotherapy (a procedure that freezes and destroys abnormal tissues) or LEEP (an electrosurgical excision procedure that utilizes an electrical current to remove abnormal tissue) are common procedures that can take place in the clinic. A CKC (cold knife conization) is another option that takes place as outpatient surgery in the hospital.
“It can take three to seven years for ‘high-grade’ or ‘severe’ abnormalities to become cervical cancer,” Dr. Anderson says. “Generally, patients are filled with anxiety when they hear ‘pre-cancerous’ cells. If they have any questions or worries, I want them to know that they can speak to me as if they are speaking to a friend.”
Board-certified in Obstetrics and Gynecology, Dr. Anderson treats women for routine gynecologic care, pregnancy and postpartum care, contraceptive choices, family planning and surgical services. “My patients are all ages, from adolescence to menopause,” she says. “I find that when women have a relationship with their OB-GYN, it creates a comfortable environment in which patients are able to communicate their health concerns/issues without fear and anxiety. This creates the foundation for good medical care.”
