Spotlight on Men’s Health
Innovative technology advances prostate cancer detection.
 Other than skin cancer, prostate cancer is the most common form of cancer and the second-leading cause of cancer death for American men. It is estimated that one in six men will be diagnosed with prostate cancer during his lifetime.
Other than skin cancer, prostate cancer is the most common form of cancer and the second-leading cause of cancer death for American men. It is estimated that one in six men will be diagnosed with prostate cancer during his lifetime.
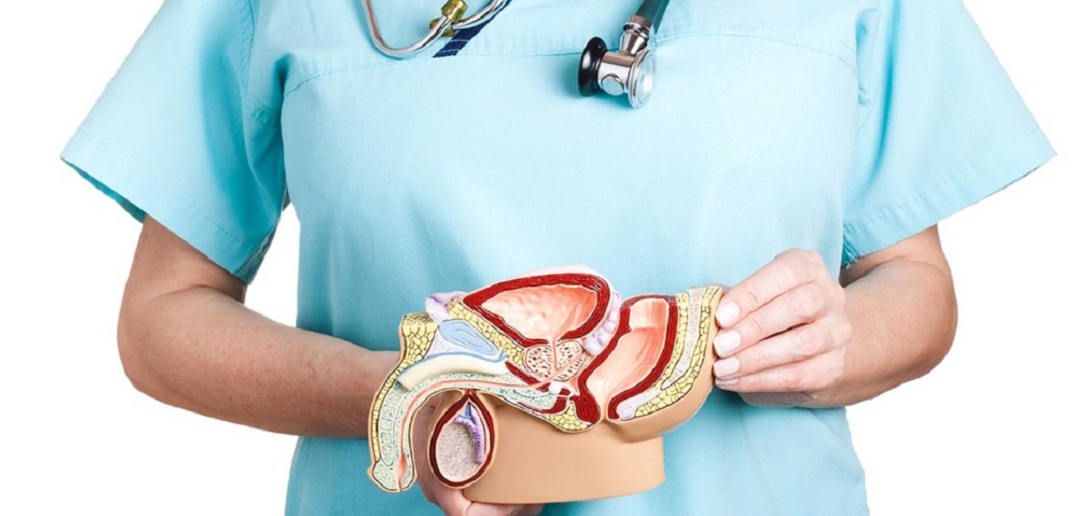
Prostate cancer forms in tissues of the prostate, a gland in the male reproductive system. Because it is a disease that grows rather slowly (occurring more frequently in older men), early detection and diagnosis is crucial to saving lives.
THE PROS AND CONS OF PSA
PSA (prostate-specific antigen) testing began in the 1980s and along with it came a significant increase in the earlier detection of prostate cancer. Because the diagnosis was often made after the cancer had metastasized (spread to other areas), this led to the over treatment of non-fatal prostate cancer. Over treatment also led to potential complications, including increased risk of impotence and incontinence.
Continuing through the 1990s, if the prostate exam revealed abnormalities, patients were treated with hormone and/or radiation therapy. The options for hormone therapy included medical or surgical castration or treatment with estrogen. Side effects of radiation therapy included complications, such as urinary incontinence, urinary leakage and impotence.
Touro’s board-certified urologist, Dr. Richard M. Vanlangendonck, Jr, explains how innovative technology — such as multiparametric MRI’s and UroNav fusion biopsies — have changed how prostate cancer is diagnosed and treated. “Up until now, we have had two methods of prostate cancer screening, prostate-specific antigen (PSA) tests and digital rectal exams (DRE),” Dr. Vanlangendonck says. “Despite the benefits of PSA-based screening, PSA levels can fluctuate for numerous reasons besides the presence of cancer. Prostate enlargement, infection and age can all affect PSA levels.”
AFTER PSA, WHAT’S NEXT
After patients undergo PSA screening or digital rectum examination, if an abnormality is seen, physicians will use an MRI and biopsy to categorize the stage of the disease and determine the best treatment. “If we find that the PSA is elevated or there is an abnormal rectal exam, we may do a regular random biopsy before discussing how to proceed,” Dr. Vanlangendonck says. “We will then look at factors such as age and whether the patient is in a high-risk group (according to race, family history, etc.) for prostate cancer and put in all the information into a prostate risk calculator. From there we will find out the percentages for finding the risk of cancer and the risk of finding a high grade of cancer.”
The second step in the conventional process for diagnosing prostate cancer was to perform a transrectal ultrasound (TRUS) biopsy. “The TRUS biopsy is one of the most reliable methods of detection, however it too presents challenges because it is difficult to visualize the entirety of the prostate as well as the location of the biopsy needle,” Dr. Vanlangendonck says. “The image resolution is sometimes poor, and, with TRUS, there is a chance that the biopsy needle will pass through a tumor-free area of the prostate and potentially miss the tumor entirely.”
In recent years, the multiparametric MRI has emerged as a more effective way to detect prostate cancer and to triage men for biopsy and guide the treatment recommendations. Radiologists can utilize multiparametric MRIs to measure the extent of a tumor, identify the location or locations of a tumor, estimate the Gleason score of a tumor and determine whether a tumor has spread beyond the prostate gland.
The new software, Invivo, “fuses” MRI scans with live, real-time ultrasound images of the prostate allowing the radiologist to review it and mark suspicious areas. “The fused image is then used to guide the biopsy needles precisely to the lesion we want to sample rather than poking around and hoping we find something,” Dr. Vanlangendonck says. “It’s like using a GPS to reach your destination rather than driving without directions. When the MRI and ultrasound images are fused, we can get an even clearer target to where to biopsy.”
TARGETED BIOPSIES
And because historically, urologists have had a difficult time distinguishing between moderate and aggressive lesions in the prostate. The UroNav fusion biopsy system is a game-changer. With UroNav, surgeons can achieve more accurate biopsies in the prostate, and, in return, more accurate diagnoses. By utilizing a tiny, navigation sensor attached to an ultrasound probe, UroNav engages a localized electromagnetic field that helps physicians determine the location of the abnormal cells. By providing better visualization and recording in multiple 2D and 3D views, the UroNav provides a better pre- and post-biopsy review.
Practicing medicine for more than 20 years, Dr. Vanlangendonck, has witnessed the extraordinary advances in the diagnosis and treatment of prostate cancer. “By combining pre-biopsy MRI images with ultrasound technology, we can better detect suspicious lesions, delineation of the prostate and clear visualization of the biopsy needle,” he says. “UroNav is a cutting-edge option for diagnosing prostate cancer. At Touro, we are committed to providing the highest quality of care to our patients, and the UroNav is poised to become a new standard in prostate care.”
Not everyone who has an abnormal prostate exam needs surgery or needs to be treated, however standard treatment options now include active surveillance, surgery, radiation therapy, hormonal therapy, chemotherapy, biologic therapy, bisphosphonate therapy and targeted therapy. These treatments can be used once or combined. If surgery is needed, Dr. Vanlangendonck utilizes state-of-the-art technology to provide his patients with the most effective, least invasive surgical treatments available. “Now with the use of robotics, we can perform minimally invasive surgery, and decrease blood loss and improve outcomes,” he says.
Dr. Richard Vanlangendonck is a urologist with Crescent City Physicians, a subsidiary of Touro Infirmary. He is board-certified by the American Board of Urology and is fellowship-trained in minimally invasive urological surgery with a primary focus on prostate and kidney cancers. Dr. Vanlangendonck sees patients for an array of urological conditions, but a great deal of his time is spent in the operating room performing robotic surgeries to treat cancer patients, having performed more than 3,000 robotic surgeries.
